|
OR Best Practices: The Time is Right for Terminal Sterilization
According to experts, there is a definite move toward terminal sterilization in the OR.1 Terminal sterilization means that a device has been processed in a system that delivers a sterility assurance level of 10-6 and is packaged in a manner that will preserve its sterility and allow it to be transferred to a sterile operating field without contamination.
Cynthia Spry, RN, MSN, MA, CNOR, co-chair of the working group responsible for the document Comprehensive Guide to Steam Sterilization and Sterility Assurance in Healthcare Facilities NASI/AAMI ST79, recently stated that the “AAMI doesn't recommend flash sterilization or just in time sterilization any more than the CDC does... It really focuses on terminal sterilization.”1
This trend toward terminal sterilization, combined with the FDA’s recent requirement that users transition from the STERIS System I* (SS1), a just-in-time processor, may provide an ideal time for facilities to upgrade their technologies to enhance their standard of care in the OR. According to Spry, with terminal sterilization, “…you decrease the risk of contaminated instruments…which is all part of patient safety goals, that is, preventing patient injury. ...Terminal sterilization is the gold standard. I can think of no reason why one shouldn't transition to it, and now is the perfect time.”1
READ MORE

IS IT STERILE? Clearing the Confusion About Liquid Chemical Sterilization
The controversy continues for hospitals using the STERIS System 1* (SS1) for “just-in-time” sterilization following the FDA mandate that hospitals transition to a legally marketed alternative. STERIS is offering a new liquid chemical sterilant processing system—the STERIS System 1E* (SS1E). At first glance, this unit might seem a viable alternative, but the use of non-sterile rinse water and the possible exposure of wet, unwrapped devices to the ambient room environment upon removal from the processor have led the FDA to conclude that devices processed in the SS1E cannot be assured to be sterile.
Non-Sterile Rinse Water
The SS1E utilizes filtration and ultraviolet (UV) irradiation to treat water used to rinse devices at the end of the sterilization phase to remove residual chemical sterilant.1 The lack of sterility assurance after rinsing recently was highlighted by the FDA:
The rinse water is tap (potable) water that has been filtered and exposed to ultraviolet rays. It is treated to minimize any bioburden that may be naturally occurring in the water. Because the rinse water is not sterile, devices processed using liquid chemical sterilization cannot be assured to be sterile.1
READ MORE
 With just-in-time sterilization, the FDA says that devices should be used “immediately.” What exactly does this mean? With just-in-time sterilization, the FDA says that devices should be used “immediately.” What exactly does this mean?
 As indicated by its name, with just-in-time sterilization, instruments must be used as soon as processing has been completed—similar to flash sterilization. For example, according to an FDA overview about the STERIS System 1E, “The processed loads should be used immediately.”1 As a result, if instruments remain in the processor upon completion of the cycle, they may need to be processed again before they can be used for procedures, potentially increasing reprocessing costs as well as the possibility of instrument damage. Unfortunately, there is no specific definition of “immediately,” and there are many different interpretations and policies. For example, some facilities state that the device must stay in the processor with the lid closed, some state that the tray can be removed and set on a counter for a specific period of time, and some state that it must be used immediately upon completion of the cycle. As a result, facilities need to carefully determine their specific policies—and be able to document them in the event of a Joint Commission audit. For more information, refer to the instructions for use for both the processor and the instruments to be processed. In addition, facilities should ask their processor representative for the specific definition of "immediately" and request an exact time frame. As indicated by its name, with just-in-time sterilization, instruments must be used as soon as processing has been completed—similar to flash sterilization. For example, according to an FDA overview about the STERIS System 1E, “The processed loads should be used immediately.”1 As a result, if instruments remain in the processor upon completion of the cycle, they may need to be processed again before they can be used for procedures, potentially increasing reprocessing costs as well as the possibility of instrument damage. Unfortunately, there is no specific definition of “immediately,” and there are many different interpretations and policies. For example, some facilities state that the device must stay in the processor with the lid closed, some state that the tray can be removed and set on a counter for a specific period of time, and some state that it must be used immediately upon completion of the cycle. As a result, facilities need to carefully determine their specific policies—and be able to document them in the event of a Joint Commission audit. For more information, refer to the instructions for use for both the processor and the instruments to be processed. In addition, facilities should ask their processor representative for the specific definition of "immediately" and request an exact time frame.
References
1. FDA. STERIS System 1E (SS1E) Liquid Chemical Sterilant—K090036. April 5, 2010. http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/
DeviceApprovalsandClearances/Recently-ApprovedDevices/ucm207489.htm
 Can common minimally invasive surgery (MIS) instrument sets, such as arthroscopy sets, be processed in the STERIS System 1E? Can common minimally invasive surgery (MIS) instrument sets, such as arthroscopy sets, be processed in the STERIS System 1E?
 The FDA states that the “SS1E should be used only for processing heat-sensitive semi-critical and critical devices that are compatible with the S40 sterilant and processing system and cannot be sterilized by other legally marketed traditional sterilization methods validated for that type of device.”1 This statement indicates that heat-stable instruments such as stainless steel items and autoclavable endocsopes should be processed using other appropriate methods, such as steam or hydrogen peroxide gas plasma—especially if those instruments must be sterile. In fact, the FDA states that, “The SS1E should NOT be used on devices that must be sterile, unless they cannot be sterilized by other legally marketed, traditional, validated sterilization methods.”1 The FDA states that the “SS1E should be used only for processing heat-sensitive semi-critical and critical devices that are compatible with the S40 sterilant and processing system and cannot be sterilized by other legally marketed traditional sterilization methods validated for that type of device.”1 This statement indicates that heat-stable instruments such as stainless steel items and autoclavable endocsopes should be processed using other appropriate methods, such as steam or hydrogen peroxide gas plasma—especially if those instruments must be sterile. In fact, the FDA states that, “The SS1E should NOT be used on devices that must be sterile, unless they cannot be sterilized by other legally marketed, traditional, validated sterilization methods.”1
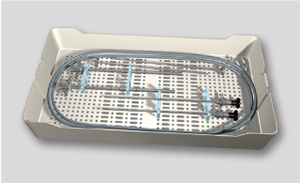
Common MIS sets, such as arthroscopy sets, were previously processed in the original SS1 and may be a concern as you look for alternative processing methods. These sets contain a variety of instruments, such as autoclavable endoscopes, stainless steel instruments, and other ancillary instrumentation that generally reflect processing options in steam or hydrogen peroxide plasma. Based on the FDA's statement about SS1E, your ability to process these sets in an SS1E may be restricted. The instruments may need to be separated, processed in different modalities, and reassembled by central processing or OR staff members. In particular, autoclavable endoscopes may need to be processed using alternative methods, such as hydrogen peroxide gas plasma or steam. Keep in mind that breaking up instrument sets may increase the likelihood that pieces may be lost, interfere with efficient workflow, and increase the risk of instrument damage in the case of steam sterilization. As an alternative, many instrument sets can be safely processed together using hydrogen peroxide gas plasma sterilization, provided the instruments meet the specific claims of the sterilizer used. This may eliminate the need to split up instrument sets and minimize the impact to your OR. Remember to follow the device manufacturer’s instructions for instrument cleaning and preparation for sterilization, which may include disassembly of removable parts (e.g., stopcocks, valves, adaptors, etc.) and proper lubrication using a water-based lubricant where required.
References
1. FDA. STERIS System 1 (SS1E) Liquid Chemical Sterilant - K090036. 2010; http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures
/DeviceApprovalsandClearances/Recently-
ApprovedDevices/ucm207489.htm. Accessed July 7, 2010.
. . . . . . . . . . . . . . . . . . . . . .
Do you have a question for Reprocessor Q&A?
E-mail us at: frontiers@aspus.jnj.com.
. . . . . . . . . . . . . . . . . . . . . .
Go Green with ASP
ASP is pleased to announce two recent developments aimed at protecting the environment:
 New packaging for CIDEX® Activated Dialdehyde Solution, available now, uses less plastic—and that means less waste, which is better for the environment. In addition, with 20% more solution in each bottle, fewer bottles are required to do the same amount of high-level disinfection, so there is less packaging to throw out. Trusted by hospitals around the world, CIDEX Activated Dialdehyde Solution provides rapid, cost-effective high-level disinfection for a wide range of endoscopes and other medical instruments. New packaging for CIDEX® Activated Dialdehyde Solution, available now, uses less plastic—and that means less waste, which is better for the environment. In addition, with 20% more solution in each bottle, fewer bottles are required to do the same amount of high-level disinfection, so there is less packaging to throw out. Trusted by hospitals around the world, CIDEX Activated Dialdehyde Solution provides rapid, cost-effective high-level disinfection for a wide range of endoscopes and other medical instruments.
IFUs for CIDEX® Activated Dialdehyde Solution (2266) and CIDEX® OPA Solution (20390) now are available online at www.e-ifu.com or via fax at the company’s FAX-On Demand System (888-783-7723), which means less printed paper and fewer trees destroyed. Over time, IFUs for more ASP products will be available on the site. The e-IFU Web site provides Johnson & Johnson customers with convenient access to IFUs and other related information anytime, anywhere. The site is easy to use—customers can browse products by company, product name, or catalog number. Visit www.e-ifu.com to learn more.
. . . . . . . . . . . . .
|
 Check Out the New ASPJJ.com Today! Check Out the New ASPJJ.com Today!
ASP launched an entirely new aspjj.com Web site with a brighter look, fresher content, and enhanced functionality to expand and improve your ability to access infection prevention resources and education.
The new aspjj.com site provides convenient, centralized access to the latest information from ASP and highlights the incredible ways ASP solutions can benefit your healthcare facility and patients, including archived presentations of ASP’s first four Webinar series installments. Now easily accessible for viewing, they showcase experiences and advice on the STERIS* System 1 transition from a cross-section of professionals ranging from operating room nurses and directors to medical device manufacturers, sterile processing experts, and microbiologists.
Check out the new aspjj.com site today!
|
. . . . . . . . . . . . .

The Spaulding Classification System
By Barbara Trattler, RN, MPA, CNOR, CAN
The Spaulding Classification System divides medical devices into categories based on the risk of infection involved with their use. The system is used to determine the degree of disinfection or sterilization required for various medical devices. It defines three categories of medical devices and their required level of disinfection or sterilization:1
- Critical—A device that enters normally sterile tissue or the vascular system. These devices should be sterilized.
- Semicritical—A device that comes into contact with intact mucous membranes and does not ordinarily penetrate sterile tissue. These devices should receive at least high-level disinfection.
- Noncritical—Devices that do not ordinarily touch the patient or touch only intact skin. These devices may be low-level disinfected.
It is important for anyone involved in instrument processing to understand the Spaulding Classification System as a guide to determining the appropriate reprocessing methods for medical devices and surgical instruments, especially in light of rapid changes in the industry. For more information, visit www.sgna.org.
References
1. Guideline for Use of High Level Disinfectants & Sterilants for Reprocessing Flexible Gastrointestinal Endoscopes. Chicago: The Society of Gastroenterology Nurses and Associates;2007.
|

